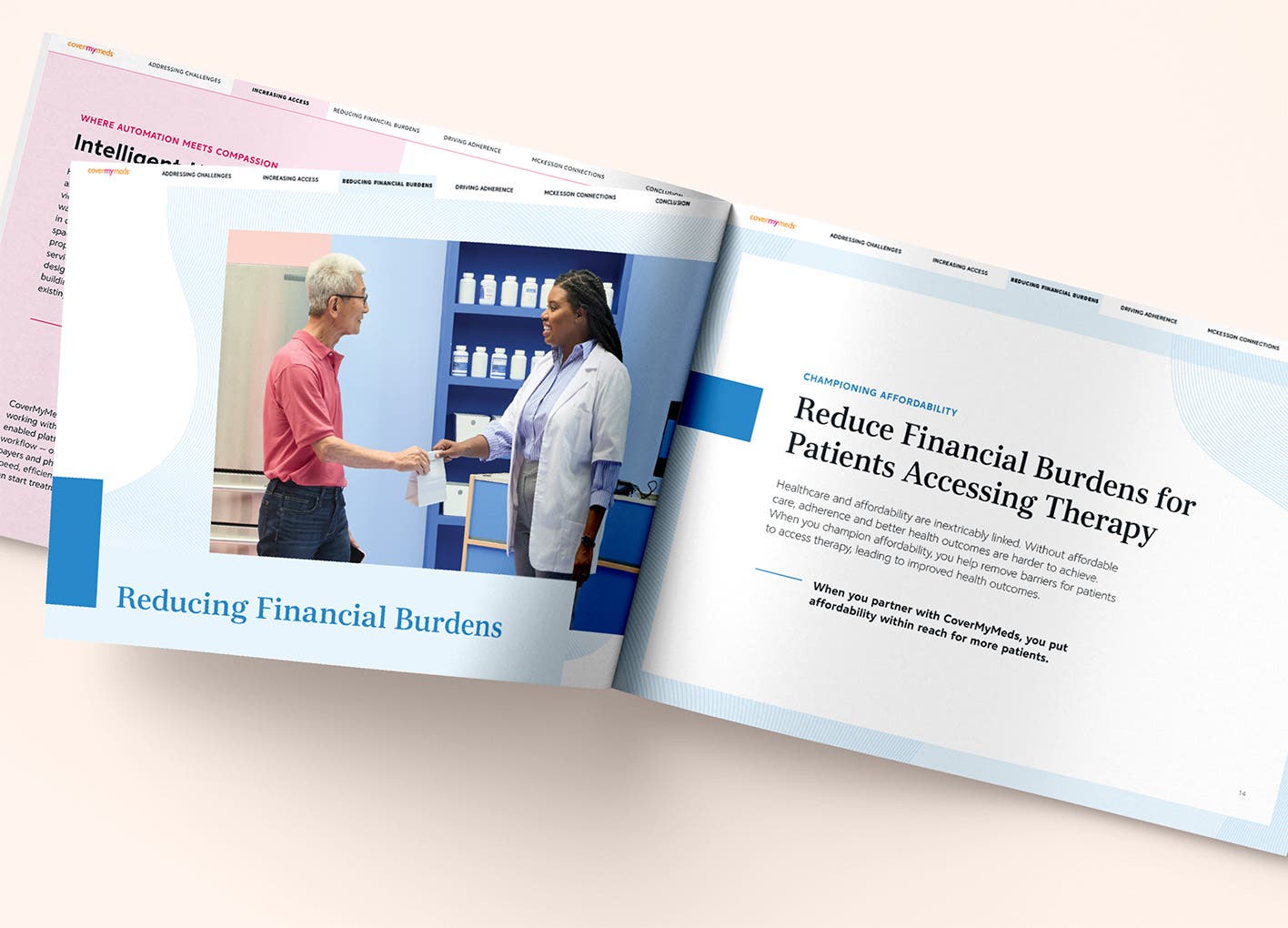
Increase patient access to care
CoverMyMeds helps patients get the treatments they need by simplifying prior authorizations.
Medication access barriers frustrate patients and hurt your brand. Discover prior auth solutions to accelerate access. Ideal for brands with high rejection rates, CoverMyMeds helps:
- In-workflow, brand-specific provider prior auth form support
- Optimized prior auth interventions on stalled requests
- Provider appeal support for denied prior auths
- Patient notification of prior auth outcome
- Data and insights related to prior auths
- On-demand provider-level data tool for field teams
Leveraging our expansive network and advanced technology, CoverMyMeds streamlines prior authorizations. This accelerates patient access to therapy. Approved patients receive their medications an average of 2.2 days sooner[0]CoverMyMeds Patient Notification data on file, 2024. Our appeal support successfully reverses denials in one out of every three cases, on average[0]Appeal support program data, 2023.
Tailor hub services to your unique patient needs. We offer flexible solutions, including provider engagement, self-service options and seamless patient enrollment.